How Lactation Works
When you get pregnant your body goes through a series of changes that start the process of making milk.
Then when your baby is born, your body really kicks into gear and revs up the milk production. You don’t even have to think about it, usually your body is just going to do its thing and *boom* your milkshakes bring your baby to your yard and they’re like, it’s better than yours…
GOOD NEWS,
your baby is going to love your milk even if you have no idea how your body works this wizardry.
Lactogenesis!
No really, that’s not some made up wizard spell word, that’s what the body’s process of making milk is actually called. Lactogenesis 1 & 2 (and some say 3 & 4).
HERE'S HOW THAT UNFOLDS...
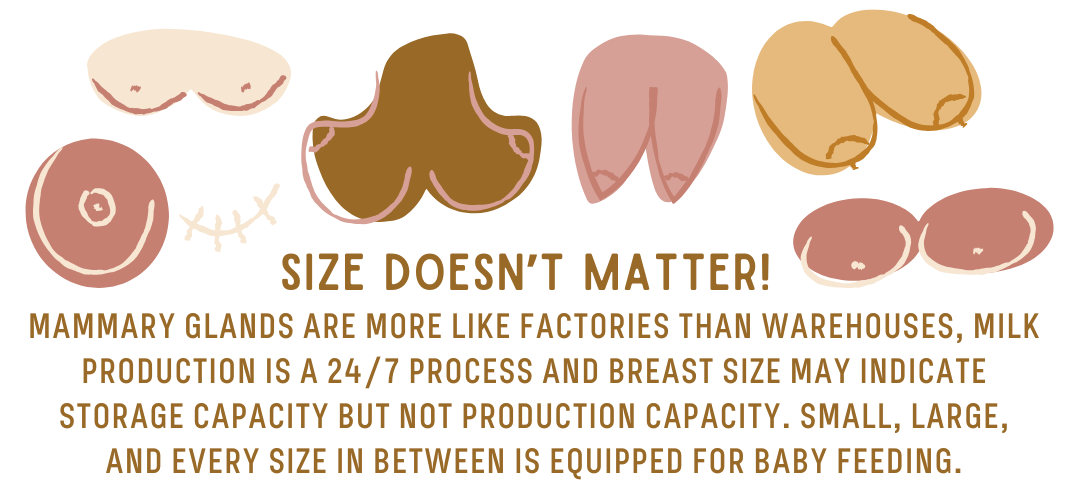
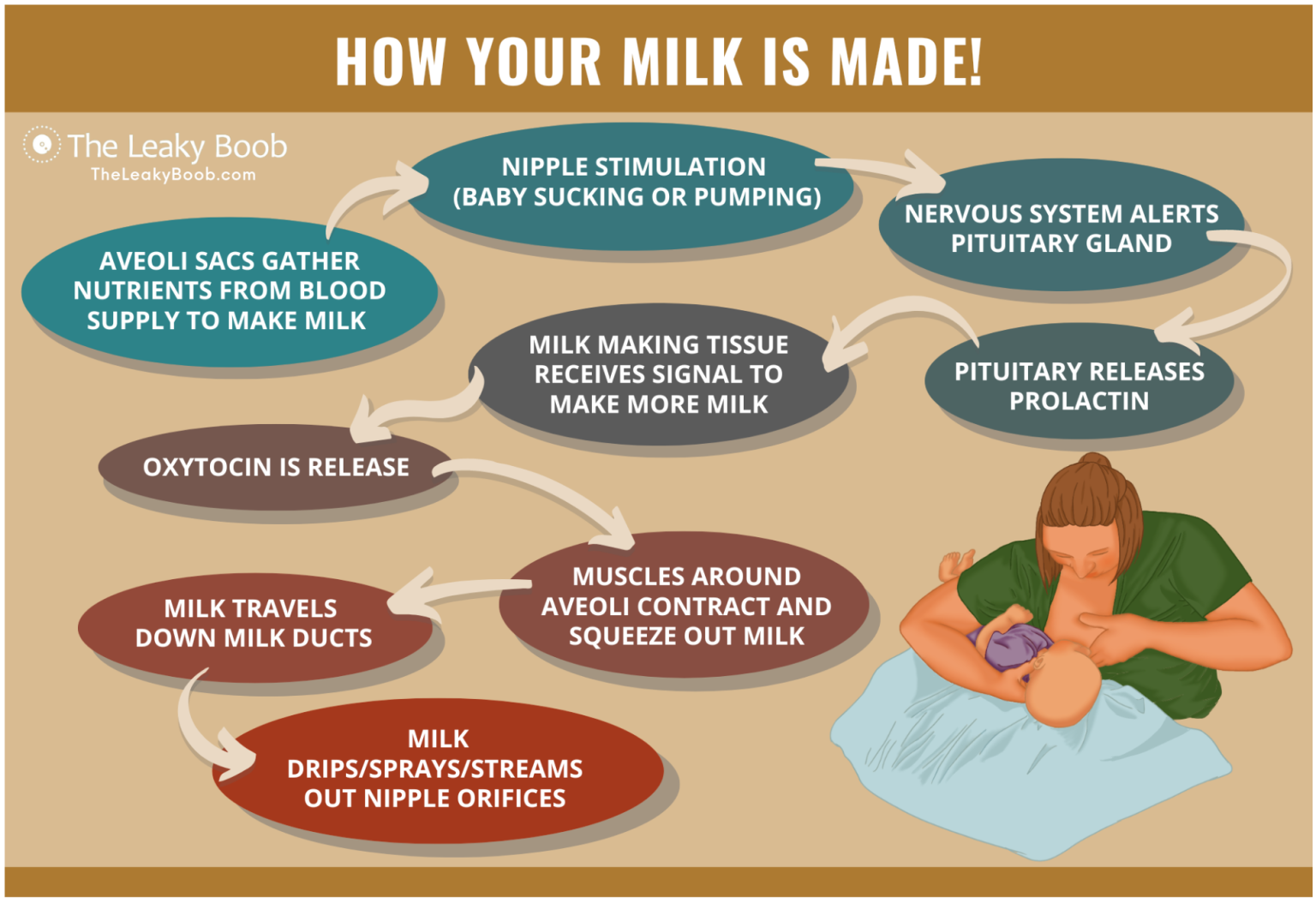
In the mammary glands (located in the breast tissue) there are grape-like clusters of cells called alveoli that respond to specific hormones called prolactin and oxytocin. Estrogen and progesterone are released during pregnancy for initial preparation for lactation (called Lactogenesis 1) and then suddenly drop with the expulsion of the placenta then prolactin and oxytocin (released in high amounts during labor) get all excited and surge which triggers a sequence for milk production (called Lactogenesis 2). Prolactin in the bloodstream moves (yes, from blood) into the alveoli and stimulates milk synthesis. Thanks to prolactin, these alveolar sacs begin to take nutrients such as protein, fat, and sugars from the blood supply and turn these nutrients into milk. Oxytocin causes the alveoli to squeeze the milk from these sacs into milk ducts, a complex system of tubes that run from the alveoli to the nipple orifices or holes to release the milk. The milk travels through the tubes and out the nipple orifices. This is called letdown.
Voilà! Milk!
Did you get all that? It sounds like a lot and this was the cliffnotes version (note: no AI here). No worries though, this all happens without having to think about it at all so if you got a little deer in the headlights… welcome to parenting.
(Don’t worry, there won’t be a quiz.)

How do we even get to this point?
The process of making milk begins long before your baby is born. The body begins laying the foundation for lactation in puberty but breasts don’t fully mature until they are producing milk. During pregnancy, rising concentrations of the hormones estrogen, progesterone cause growth and development of mammary tissue with glandular or ductal development to prepare for lactation. This change happens with every pregnancy so your lactation experience can vary greatly from one to the next as you have more milk-making tissue through this process.
Sometime between weeks 16-22 in pregnancy, the body begins to produce colostrum, a concentrated, nutrient-dense, high calorie, sticky, golden-colored first milk that has everything your baby’s tiny tummy needs for the first 3-5 days until your milk transitions to more mature full milk. Initially milk production is automatic, triggered by hormones in pregnancy to grow more milk-making tissue and kicking into full gear with the release of the placenta after giving birth.
The milk produced in pregnancy isn’t typically enough to sustain a baby unless milk production is already established, such as if you already had a baby and were breastfeeding them and continued to do so while pregnant.
Don’t freak out, we’re not even at lactogenesis 2 yet, the milk is coming.
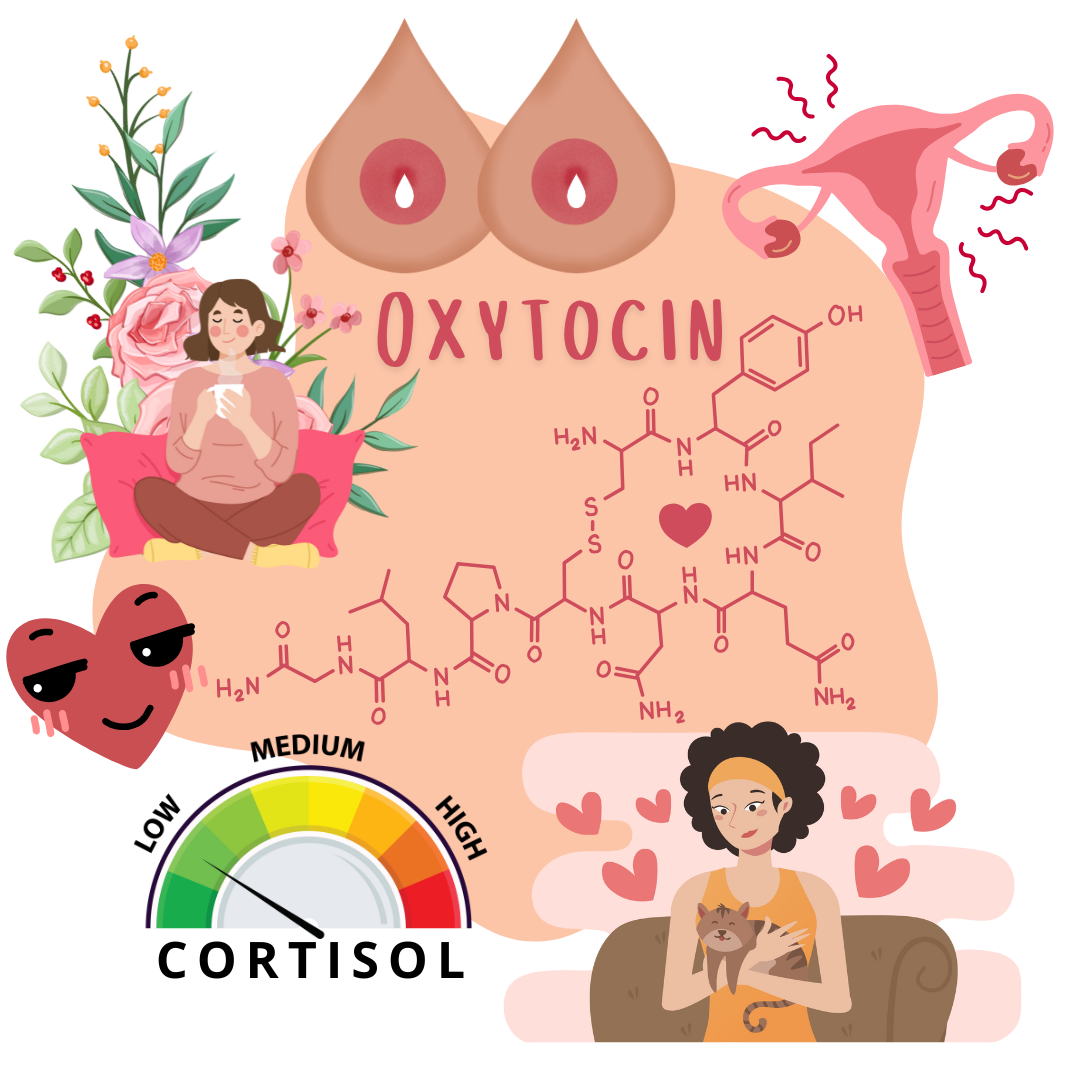
First, we're going to need some OXYTOCIN.
In labor and birth, oxytocin is released. Oxytocin is sometimes called the love hormone or the feel-good hormone but obviously only by someone that hasn’t experienced their uterus involuntarily flexing up to 60 pounds of pressure in a contraction thanks to oxytocin.
Oxytocin is responsible for uterine contractions, connected to sexual pleasure and attachment bonding, positive feelings, relaxation, lower stress levels, and the release of milk from the breast. The release of the placenta from the uterine wall triggers a sharp drop of progesterone which signals the body to produce and release prolactin from the pituitary gland. Prolactin drives milk production at first and oxytocin cues the release of milk with the let-down reflex. With nipple stimulation (baby suckling or with pumping), the body gets the alert to produce milk and let the milk flow, allowing the baby to remove milk from the breast which in turn reminds the body to make more milk for the baby for the next feed.
Initially, milk production is entirely because of hormones but this will shift in time as milk supply is established (meaning the body has gotten the message for how many babies it is feeding and how much milk to make) and milk removal will regulate production.
Click here for our Lactation Plan Template
This works thanks to a tiny whey protein found in human milk called Feedback Inhibitor of Lactation or FIL. This protein controls milk production by slowing the milk making process when the breasts remain full of milk. Without milk removal, when milk is left sitting in the breasts, FIL tells the body to slow its roll in producing milk. With regular and adequate milk removal, when there is less milk left in the breast, FIL tells the body to pick up the pace and make more milk.
Ongoing production of the hormones prolactin and oxytocin is encouraged by regular milk removal, and lactation becomes a “use it or lose it” process. The amount of Feedback Inhibitor of Lactation is higher the more milk is in the breast, it is at the lowest amount when milk has just been removed. Insufficient milk removal, frequent or repeated instances of missed feeds or other milk removal, or repeated encouragement without removing milk can cause milk production to decline over time and may contribute to low milk supply. More frequent and regular removal lowers the presence of FIL and helps ensure a robust milk supply.

Frequent suckling activates more prolactin receptors and the more prolactin receptors, the more secure the milk supply!
Feeding regularly and frequently is the first step in ensuring an adequate milk supply. For this reason, learning as much as you can about lactation and communicating your infant feeding goals with your health care providers and personal support may be a key factor in reaching your baby feeding goals. Breastfeeding classes, support groups, videos, books, and articles along with social media communities are resources that many find helpful in making informed decisions about baby feeding and preparing to nurse a new baby. Identifying your lactation goals and making a plan which you can then communicate with your support community and care providers, including your birth team, is a great step toward getting off to the best start possible with your baby feeding goals.
You may feel like all you do is nurse in the first several weeks. This is common!